Discover 5 ways to optimize IVF transfer dates, including embryo grading, uterine preparation, and hormonal balance, to increase fertility success rates and achieve a healthy pregnancy through in vitro fertilization techniques and reproductive medicine advancements.
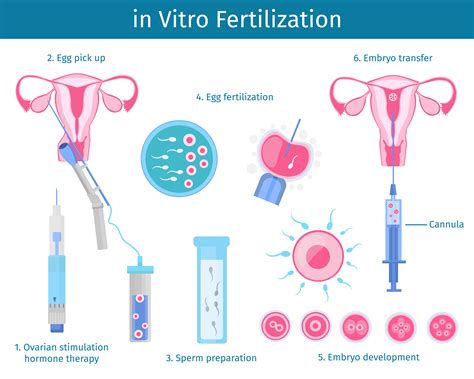
The journey to parenthood can be a long and winding road for many individuals and couples, with various twists and turns that can test patience, emotional resilience, and financial resources. Among the array of fertility treatments available, In Vitro Fertilization (IVF) stands out as a beacon of hope for those struggling with infertility. IVF involves fertilizing an egg with sperm outside the body, in a laboratory dish, and then transferring the embryo(s) into the woman's uterus. One of the most critical aspects of the IVF process is the embryo transfer, which requires precise timing to maximize the chances of a successful pregnancy. In this article, we will delve into the intricacies of the IVF transfer date, exploring the factors that influence its scheduling and the strategies employed to optimize outcomes.
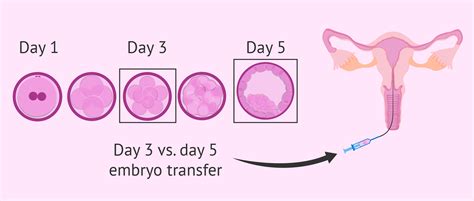
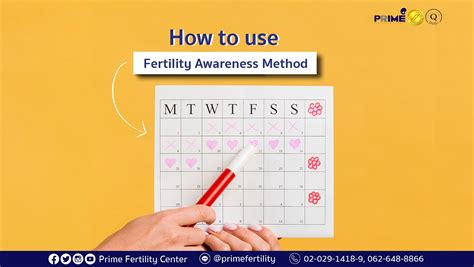
The importance of timing in IVF cannot be overstated. The human body operates on a finely tuned schedule, with hormonal fluctuations and uterine receptivity playing pivotal roles in the success of an IVF cycle. The transfer date is determined based on the development stage of the embryos and the preparation of the uterine lining. Embryos can be transferred at various stages, including the cleavage stage (typically 3 days after fertilization) and the blastocyst stage (5-6 days after fertilization). Each stage has its advantages, and the choice often depends on the quality of the embryos, the age of the woman, and previous IVF experiences.
As we navigate the complexities of IVF and the significance of the transfer date, it becomes apparent that this process is not just about medical science; it's also deeply personal and emotional. The anticipation, hope, and sometimes disappointment that accompany each step of the journey can be overwhelming. Therefore, understanding the factors that influence the IVF transfer date and the methods used to determine the optimal timing is crucial for managing expectations and making informed decisions.
Understanding IVF Transfer Dates
Understanding the IVF transfer date involves grasping the embryonic development stages and how they align with the uterine preparation. The uterine lining must be ready to receive the embryo, which typically happens after a series of hormonal treatments designed to thicken the lining and make it receptive. The embryo transfer is usually scheduled based on the type of cycle (natural, stimulated, or frozen-thawed) and the embryo's developmental stage. For instance, in a natural cycle, the transfer might be timed to coincide with the woman's natural ovulation, while in a stimulated cycle, medications control the timing.
Factors Influencing IVF Transfer Dates
Several factors can influence the scheduling of an IVF transfer date, including the woman's age, the quality and number of embryos available, previous IVF attempts, and the specific IVF protocol being used. The age of the woman is particularly significant because it affects the quality and quantity of eggs, with older women typically having fewer and less viable eggs. The quality of the embryos is another crucial factor, as higher-quality embryos have better chances of implantation and successful pregnancy.Types of IVF Transfer Cycles

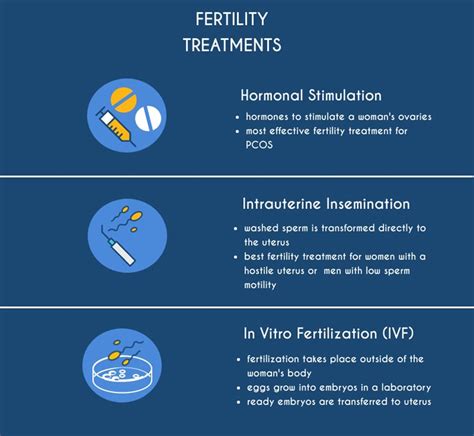
IVF transfer cycles can be broadly categorized into natural cycles, stimulated cycles, and frozen-thawed cycles. Natural cycles rely on the woman's natural hormonal fluctuations to time the transfer, stimulated cycles use medications to control ovulation and prepare the uterine lining, and frozen-thawed cycles involve thawing previously frozen embryos for transfer. Each type of cycle has its advantages and is chosen based on the individual's or couple's specific circumstances, such as the presence of regular menstrual cycles, the risk of ovarian hyperstimulation syndrome (OHSS), and the availability of frozen embryos from previous cycles.
Preparation for IVF Transfer
Preparation for the IVF transfer involves both physical and emotional components. Physically, the woman may undergo a series of medications to prepare her uterine lining and control ovulation. This preparation phase can be demanding, requiring strict adherence to medication schedules and regular monitoring through ultrasound and blood tests. Emotionally, couples may benefit from counseling or support groups to manage the stress and uncertainty of the IVF process.Strategies to Optimize IVF Transfer Outcomes

Several strategies can be employed to optimize IVF transfer outcomes. These include selecting the best quality embryos for transfer, using techniques like assisted hatching to aid implantation, and ensuring the uterine lining is adequately prepared. Lifestyle modifications, such as maintaining a healthy diet, avoiding alcohol and tobacco, and managing stress, can also contribute to a successful outcome. Furthermore, advances in genetic testing, like preimplantation genetic testing for aneuploidy (PGT-A), can help identify chromosomally normal embryos, thereby increasing the chances of a successful pregnancy.
Embryo Transfer Techniques
The technique used for embryo transfer can also impact the success rate of IVF. The transfer is typically performed under ultrasound guidance to ensure the embryos are placed in the optimal position within the uterus. The use of a soft catheter and a full bladder (to help visualize the uterus on ultrasound) are common practices. Additionally, studies have shown that techniques like embryo glue, which mimics the natural molecules that help embryos implant, and the use of a medium that supports embryo development during the transfer, may enhance implantation rates.Managing Expectations and Emotional Well-being

The emotional journey of IVF is just as significant as the medical process. Managing expectations and maintaining emotional well-being are crucial for navigating the highs and lows of treatment. Support from partners, family, friends, and professional counselors can be invaluable. Additionally, engaging in stress-reducing activities, such as meditation, yoga, or other mindfulness practices, can help individuals cope with the uncertainty and potential disappointment that may arise during the IVF process.
Coping with IVF Outcomes
The outcome of an IVF cycle can be a significant source of stress and emotional upheaval. A positive pregnancy test can bring immense joy, while a negative result can lead to disappointment and frustration. It's essential to remember that each IVF cycle provides valuable information that can be used to adjust and improve subsequent attempts. Couples should discuss their feelings, concerns, and future plans with their healthcare provider, who can offer guidance and support based on their specific situation.Future Directions in IVF

The field of IVF is continuously evolving, with ongoing research and technological advancements aimed at improving success rates and expanding access to fertility treatments. Future directions include the development of more sophisticated genetic testing methods, improvements in embryo culture mediums, and the exploration of novel stimulation protocols that minimize side effects and maximize egg quality. Additionally, there is a growing interest in personalized medicine approaches, where treatments are tailored to the individual's unique genetic, hormonal, and reproductive profile.
Access to IVF and Equity in Fertility Care
Despite the advancements in IVF, access to fertility care remains a significant challenge for many individuals and couples worldwide. Barriers such as cost, insurance coverage, and geographic location can limit access to these life-changing treatments. Efforts to address these disparities and promote equity in fertility care are essential, including advocacy for insurance coverage, sliding scale fee structures, and the development of more affordable treatment options without compromising quality.IVF Image Gallery





As we conclude our exploration of the IVF transfer date and its significance in the journey to parenthood, it's clear that this process is multifaceted, involving not just medical science, but also emotional resilience, financial planning, and personal commitment. By understanding the factors that influence the IVF transfer date, the strategies to optimize outcomes, and the ongoing advancements in the field, individuals and couples can better navigate their fertility journey. We invite you to share your thoughts, experiences, and questions about IVF and fertility treatments in the comments below, and to consider sharing this article with others who may be embarking on or considering their own fertility journey. Together, we can foster a supportive community that encourages open dialogue, promotes awareness, and celebrates the diverse paths to building a family.
