Intro
Master the Gestational Diabetes ATi Template with our comprehensive guide. Learn how to identify high-risk patients, understand diagnostic criteria, and develop personalized care plans. Stay up-to-date on the latest treatment options and management strategies for gestational diabetes, including nutrition therapy, insulin administration, and glucose monitoring.
Gestational diabetes is a type of diabetes that develops during pregnancy, typically in the second or third trimester. It is a significant health concern for pregnant women, as it can pose risks to both the mother and the baby. Understanding gestational diabetes, its causes, symptoms, diagnosis, treatment, and management is crucial for expecting mothers to ensure a healthy pregnancy and delivery.
Understanding Gestational Diabetes
Gestational diabetes is a condition characterized by high blood sugar levels during pregnancy. It is caused by the placenta producing hormones that block the action of insulin, a hormone that regulates blood sugar levels. As a result, the body either cannot produce enough insulin or cannot effectively use the insulin it produces.
Risk Factors for Gestational Diabetes
Certain factors increase a woman's risk of developing gestational diabetes. These include:
- Being overweight or obese
- Having a family history of diabetes
- Having had gestational diabetes in a previous pregnancy
- Having given birth to a large baby (over 9 pounds)
- Being over 35 years old
- Having a history of delivering a stillborn baby or a baby with birth defects
- Having high blood pressure or high cholesterol
- Being of African American, Hispanic/Latina, American Indian, or Asian American ethnicity
Causes and Symptoms of Gestational Diabetes
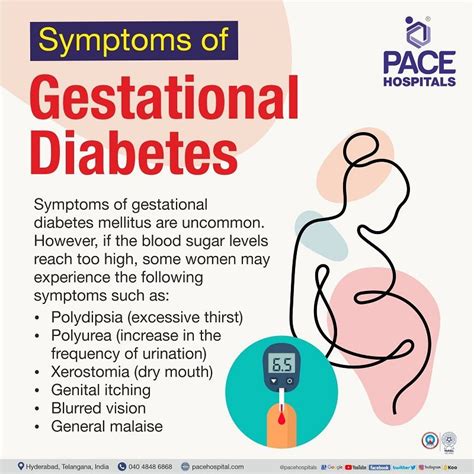
The exact cause of gestational diabetes is still unknown, but it is believed to be related to the hormonal changes that occur during pregnancy. The symptoms of gestational diabetes can be mild and may not always be noticeable. However, some common symptoms include:
- Increased thirst and urination
- Fatigue
- Blurred vision
- Cuts or wounds that are slow to heal
- Frequent infections, such as yeast infections or UTIs
Diagnosis and Testing for Gestational Diabetes
Gestational diabetes is typically diagnosed between 24 and 28 weeks of pregnancy using a two-step testing process:
- Glucose Screening Test: This test measures the level of glucose in the blood after consuming a sugary drink.
- Glucose Tolerance Test: This test measures the level of glucose in the blood after consuming a sugary drink and then again after a period of time (usually 1-2 hours).
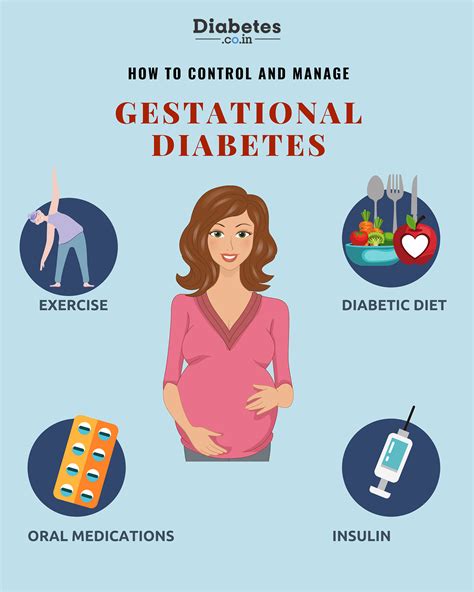
Treatment and Management of Gestational Diabetes
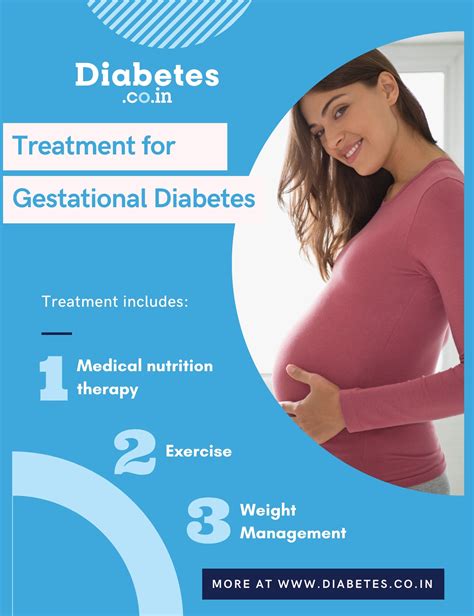
Treatment for gestational diabetes usually involves a combination of lifestyle changes and medication. Lifestyle changes may include:
- Eating a healthy, balanced diet that is low in sugar and refined carbohydrates
- Engaging in regular physical activity, such as walking or swimming
- Monitoring blood sugar levels regularly
- Maintaining a healthy weight
In some cases, medication may be necessary to control blood sugar levels. This may include insulin or oral medications.
Complications of Gestational Diabetes
If left untreated or poorly managed, gestational diabetes can pose serious health risks to both the mother and the baby. Complications may include:
- High blood pressure and preeclampsia
- Premature birth
- Birth defects
- Stillbirth
- Macrosomia (giving birth to a large baby)
- Increased risk of cesarean delivery
Managing Gestational Diabetes
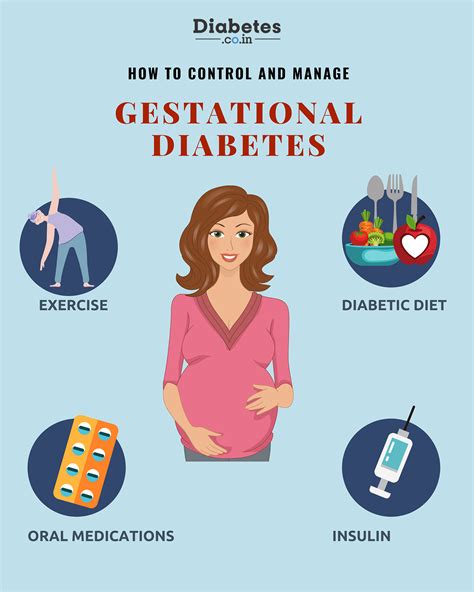
Managing gestational diabetes requires a multidisciplinary approach that involves the healthcare provider, a registered dietitian, and the expecting mother. Key components of management include:
- Regular prenatal care and monitoring
- Healthy eating habits
- Regular physical activity
- Monitoring blood sugar levels
- Medication (if necessary)
Lifestyle Changes for Managing Gestational Diabetes
Making healthy lifestyle changes can help manage gestational diabetes and reduce the risk of complications. These changes may include:
- Eating a healthy, balanced diet that is low in sugar and refined carbohydrates
- Engaging in regular physical activity, such as walking or swimming
- Maintaining a healthy weight
- Getting enough sleep
- Managing stress
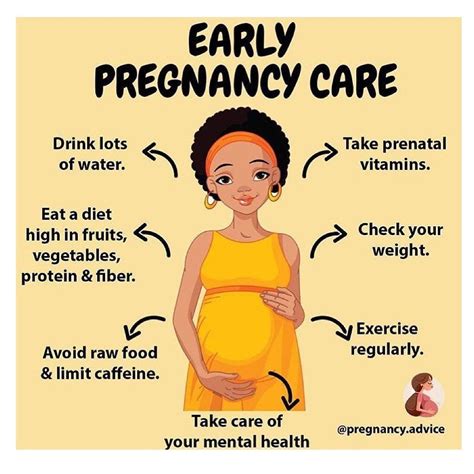
Gestational Diabetes Image Gallery









By understanding gestational diabetes and taking proactive steps to manage it, expecting mothers can reduce the risk of complications and ensure a healthy pregnancy and delivery. If you have any concerns about gestational diabetes or would like to learn more, please share your thoughts in the comments section below.
