Intro
Master hidradenitis management with expert tips, treating symptoms, and preventing flare-ups, using natural remedies, skincare routines, and medical treatments for effective hidradenitis suppuration control and relief.
Hidradenitis suppurativa, commonly referred to as hidradenitis, is a chronic skin condition characterized by the occurrence of inflamed and painful lesions, particularly in areas of the body where skin folds occur, such as the armpits, groin, and under the breasts. This condition can significantly impact an individual's quality of life, causing discomfort, embarrassment, and difficulty with daily activities. Understanding the importance of managing hidradenitis is crucial for those affected, as it can help alleviate symptoms, prevent complications, and improve overall well-being.
The importance of hidradenitis management cannot be overstated. Effective management involves a combination of medical treatments, lifestyle modifications, and self-care practices. It requires a comprehensive approach that addresses not only the physical aspects of the condition but also its psychological and emotional impacts. By adopting a proactive and informed approach to managing hidradenitis, individuals can better control their symptoms, reduce the risk of infections and other complications, and enhance their ability to engage in daily activities without hindrance.
For individuals living with hidradenitis, finding the right management strategies can be a process of trial and error. What works for one person may not work for another, making it essential to work closely with healthcare professionals to develop a personalized treatment plan. This plan may include medications to reduce inflammation and prevent infections, surgical interventions for advanced cases, and lifestyle changes such as maintaining good hygiene, wearing loose clothing, and quitting smoking. Additionally, understanding the triggers of hidradenitis flares, such as stress, tight clothing, and certain foods, can help individuals make informed choices to minimize their occurrence.
Hidradenitis Overview

Hidradenitis suppurativa is a complex condition that affects a significant portion of the population worldwide. Despite its prevalence, there is a lack of awareness about hidradenitis, leading to delays in diagnosis and treatment. The condition is characterized by recurrent, painful abscesses and nodules in apocrine-gland-bearing areas of the body. These lesions can rupture and lead to the formation of tunnels under the skin, known as fistulas, and scarring. The exact cause of hidradenitis is not fully understood, but it is believed to involve a combination of genetic, hormonal, and environmental factors.
Causes and Risk Factors
The development of hidradenitis is thought to be influenced by several factors, including genetics, obesity, smoking, and hormonal changes. Individuals with a family history of the condition are at a higher risk, suggesting a genetic component. Additionally, factors such as friction, pressure, and humidity in skin folds can contribute to the onset of hidradenitis. Understanding these causes and risk factors is essential for developing effective prevention and management strategies.Hidradenitis Symptoms and Diagnosis

The symptoms of hidradenitis can vary in severity and impact. Common symptoms include painful lumps or abscesses in the affected areas, pus or fluid discharge, and a foul odor. As the condition progresses, individuals may experience recurring episodes of inflammation, scarring, and the formation of tunnels or fistulas under the skin. Diagnosis is typically based on a physical examination and medical history. In some cases, a biopsy may be performed to rule out other conditions.
Stages of Hidradenitis
Hidradenitis suppurativa is categorized into three stages based on its severity. The first stage is characterized by occasional abscesses and single or multiple, widely separated lesions without scarring. The second stage involves recurrent abscesses, single or multiple, widely separated lesions with some scarring, and possibly fistulas. The third and most severe stage is marked by extensive tunnelling, abscesses, and scarring across the entire affected area. Understanding the stage of hidradenitis is crucial for determining the appropriate treatment approach.Treatment Options for Hidradenitis

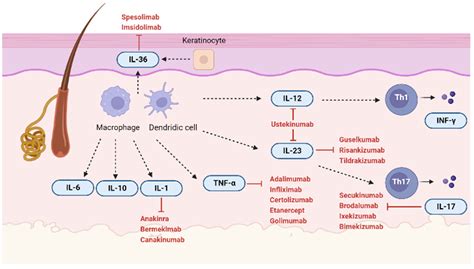
The management of hidradenitis involves a range of treatments, from topical and oral medications to surgical interventions. Topical antibiotics and retinoids can help reduce inflammation and prevent bacterial infections. For more severe cases, oral antibiotics, corticosteroids, and biologics may be prescribed. In advanced stages, surgical procedures such as incision and drainage, debridement, or excision may be necessary to remove affected tissue and promote healing.
Lifestyle Modifications
In addition to medical treatments, lifestyle modifications play a crucial role in managing hidradenitis. Maintaining good hygiene, wearing loose, comfortable clothing, and avoiding tight-fitting garments can help reduce friction and irritation. Quitting smoking and managing weight can also alleviate symptoms. Stress management techniques, such as meditation and exercise, can help reduce the psychological impact of the condition.Complications and Prevention
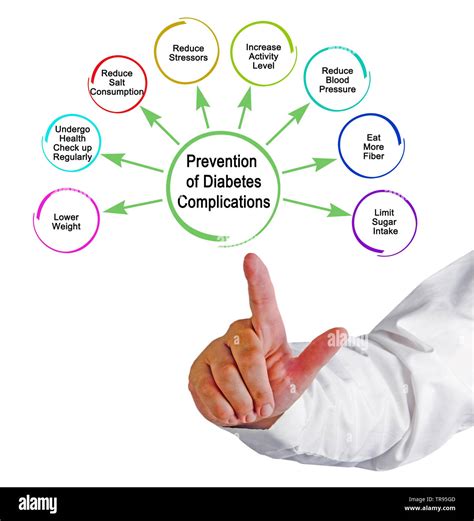
If left untreated or poorly managed, hidradenitis can lead to several complications, including infections, scarring, and the development of fistulas. Emotional and psychological distress, such as anxiety and depression, are also common among individuals with hidradenitis. Preventive measures, such as good hygiene practices, regular check-ups with healthcare providers, and adherence to treatment plans, can help mitigate these risks.
Psychological Impact
The psychological impact of hidradenitis should not be underestimated. The condition can lead to feelings of embarrassment, low self-esteem, and social isolation. Support from family, friends, and support groups can be invaluable in coping with these challenges. Mental health professionals can also provide strategies and therapies to manage the emotional aspects of living with hidradenitis.Future Directions in Hidradenitis Management

Research into hidradenitis is ongoing, with a focus on understanding its causes, developing more effective treatments, and improving patient outcomes. Advances in biologic therapies and surgical techniques offer promising avenues for managing the condition. Additionally, there is a growing recognition of the importance of addressing the psychological and social impacts of hidradenitis, highlighting the need for a holistic approach to care.
Conclusion and Next Steps
In conclusion, managing hidradenitis requires a comprehensive and personalized approach that encompasses medical treatments, lifestyle modifications, and emotional support. By understanding the condition, its symptoms, and the available treatment options, individuals can take proactive steps towards improving their quality of life. It is essential to work closely with healthcare providers to develop a management plan that addresses the unique needs and circumstances of each individual.Hidradenitis Management Image Gallery





We invite you to share your experiences and questions about hidradenitis management in the comments below. Your insights can help others understand the condition better and find the support they need. If you found this article informative, please consider sharing it with others who might benefit from this comprehensive guide to hidradenitis management. Together, we can raise awareness and promote a better understanding of this complex condition.
