Intro
Create comprehensive and accurate patient assessments with our guide to the 5 essential components of an OB GYN History and Physical (H&P) template. Learn how to effectively document patient histories, physical exams, diagnoses, and treatment plans, ensuring thorough and compliant documentation for obstetric and gynecologic care.
A comprehensive and well-structured Obstetrics and Gynecology (OB-GYN) History and Physical (H&P) template is essential for healthcare providers to accurately assess and diagnose patients. A good template should include the following five essential components to ensure that all relevant information is collected and documented.
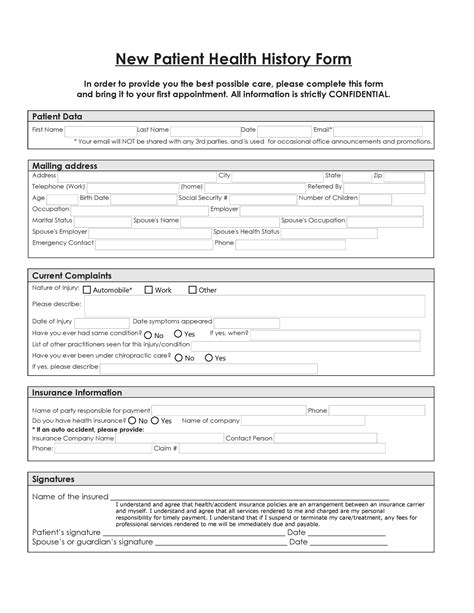
Component 1: Patient Demographics and Chief Complaint
The patient demographics section should include the patient's name, age, date of birth, and contact information. The chief complaint section should document the patient's primary reason for seeking medical attention, including the onset, duration, and severity of symptoms. This information provides context for the rest of the H&P and helps healthcare providers focus on the most critical issues.
Key Elements:
- Patient's name and contact information
- Date of birth and age
- Chief complaint, including onset, duration, and severity of symptoms
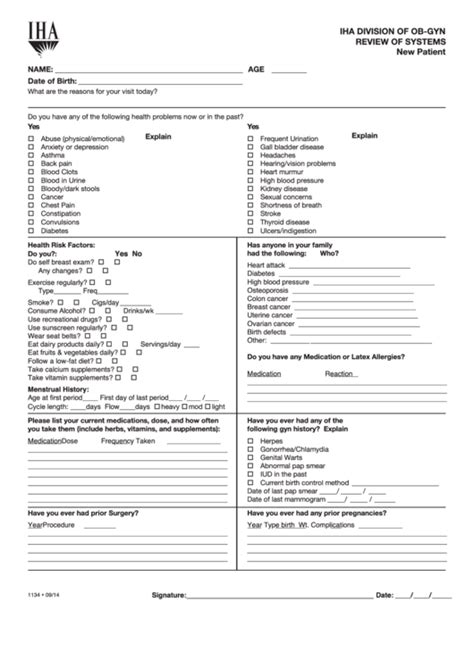
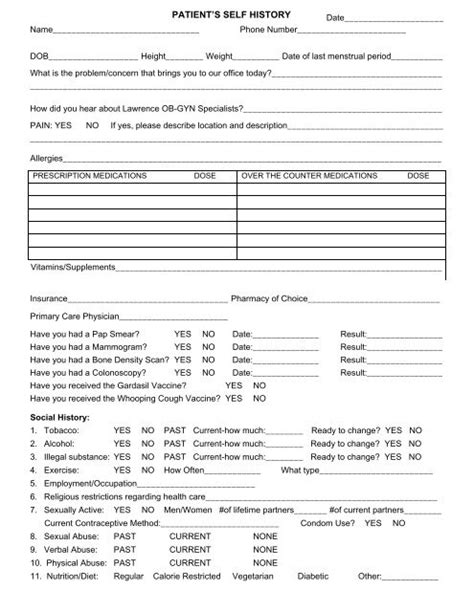
Component 2: Medical and Surgical History
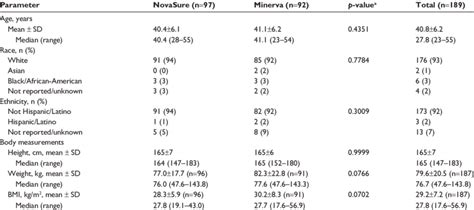
A thorough medical and surgical history is crucial for identifying potential health risks and complications. This section should include the patient's:
- Medical conditions, such as hypertension, diabetes, or thyroid disease
- Surgical history, including cesarean sections, hysterectomies, or other relevant procedures
- Allergies and sensitivities to medications or substances
- Current medications and dosages
Key Elements:
- Medical conditions and their management
- Surgical history, including dates and procedures
- Allergies and sensitivities
- Current medications and dosages
Component 3: Obstetric and Gynecologic History
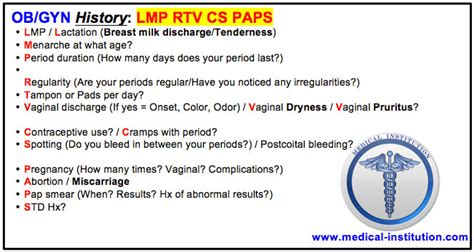
The obstetric and gynecologic history section should document the patient's reproductive health, including:
- Menstrual history, including the date of the last menstrual period (LMP) and menstrual flow
- Pregnancy history, including the number of pregnancies, deliveries, and miscarriages
- Gynecologic surgeries, such as tubal ligations or hysterectomies
- History of infertility or recurrent pregnancy loss
Key Elements:
- Menstrual history, including LMP and menstrual flow
- Pregnancy history, including number of pregnancies, deliveries, and miscarriages
- Gynecologic surgeries and procedures
- History of infertility or recurrent pregnancy loss
Component 4: Physical Examination

The physical examination section should document the patient's vital signs, including temperature, blood pressure, and pulse. The examination should also include an assessment of the:
- Abdomen, including any masses or tenderness
- Pelvic organs, including the cervix, uterus, and ovaries
- Breasts, including any masses or abnormalities
Key Elements:
- Vital signs, including temperature, blood pressure, and pulse
- Abdominal examination, including any masses or tenderness
- Pelvic examination, including the cervix, uterus, and ovaries
- Breast examination, including any masses or abnormalities
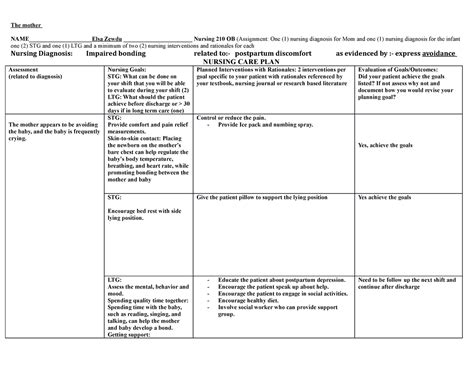
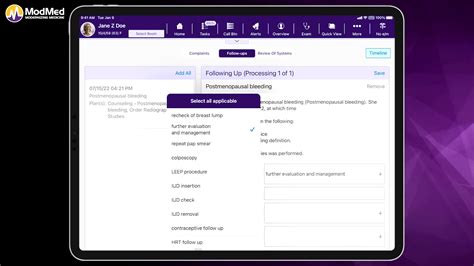
Component 5: Assessment and Plan
The assessment and plan section should summarize the patient's diagnosis and treatment plan. This section should include:
- A diagnosis or differential diagnosis
- A treatment plan, including medications, procedures, or referrals
- Follow-up instructions, including any necessary testing or appointments
Key Elements:
- Diagnosis or differential diagnosis
- Treatment plan, including medications, procedures, or referrals
- Follow-up instructions, including any necessary testing or appointments
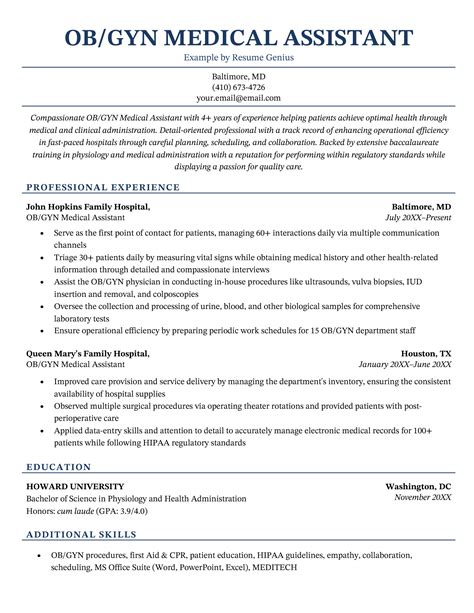
OB-GYN History and Physical Template Image Gallery



In conclusion, a comprehensive OB-GYN H&P template is essential for healthcare providers to accurately assess and diagnose patients. The five essential components of a well-structured template include patient demographics and chief complaint, medical and surgical history, obstetric and gynecologic history, physical examination, and assessment and plan. By including these components, healthcare providers can ensure that they are collecting and documenting all relevant information to provide high-quality patient care.
We hope this article has provided you with a comprehensive understanding of the essential components of an OB-GYN H&P template. If you have any questions or comments, please feel free to share them below.
