Intro
Streamline your clinical documentation with our comprehensive soap note template for healthcare professionals. Learn how to efficiently chart patient information, including subjective and objective data, assessment, and treatment plans. Improve patient care and compliance with our easy-to-use template, designed for nurses, doctors, and therapists.
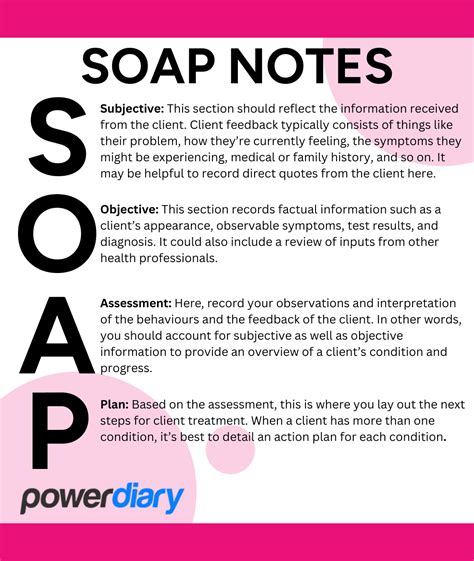
The SOAP note template is a widely used documentation tool in the healthcare industry, designed to help healthcare professionals efficiently and effectively document patient information. The SOAP note template is an acronym that stands for Subjective, Objective, Assessment, and Plan, which are the four main components of the template.
The SOAP note template is essential for healthcare professionals as it provides a standardized format for documenting patient information, which helps to ensure that all relevant information is captured and communicated effectively. In this article, we will delve into the world of SOAP note templates, exploring their importance, benefits, and how to use them effectively.
Importance of SOAP Note Templates
The SOAP note template is a crucial tool in the healthcare industry, and its importance cannot be overstated. Here are some reasons why SOAP note templates are essential for healthcare professionals:
- Improved patient care: SOAP note templates help healthcare professionals to document patient information accurately and efficiently, which enables them to provide better care and make informed decisions.
- Enhanced communication: SOAP note templates facilitate effective communication among healthcare professionals, ensuring that all team members are on the same page and that patient information is shared accurately.
- Reduced errors: SOAP note templates help to reduce errors by providing a standardized format for documenting patient information, which minimizes the risk of miscommunication and mistakes.
- Increased efficiency: SOAP note templates save time and effort by providing a structured format for documenting patient information, which enables healthcare professionals to focus on providing care rather than documenting.
Benefits of SOAP Note Templates
SOAP note templates offer numerous benefits for healthcare professionals, including:
- Improved documentation: SOAP note templates provide a standardized format for documenting patient information, which ensures that all relevant information is captured and communicated effectively.
- Enhanced patient safety: SOAP note templates help to reduce errors and improve patient safety by providing a structured format for documenting patient information.
- Increased productivity: SOAP note templates save time and effort by providing a standardized format for documenting patient information, which enables healthcare professionals to focus on providing care rather than documenting.
- Better communication: SOAP note templates facilitate effective communication among healthcare professionals, ensuring that all team members are on the same page and that patient information is shared accurately.
How to Use SOAP Note Templates
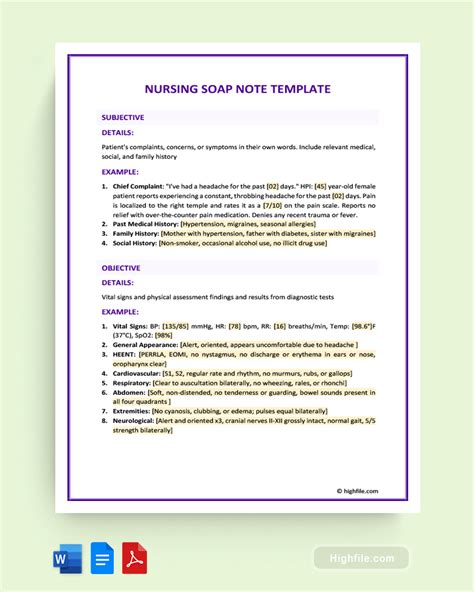
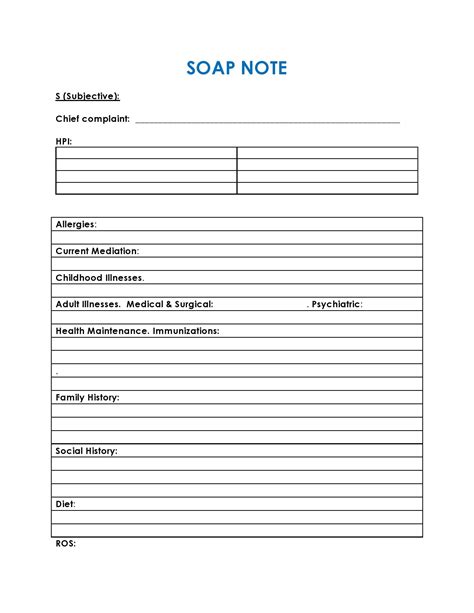
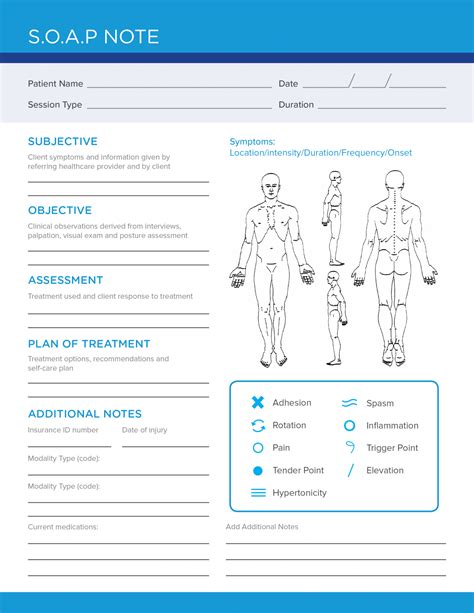
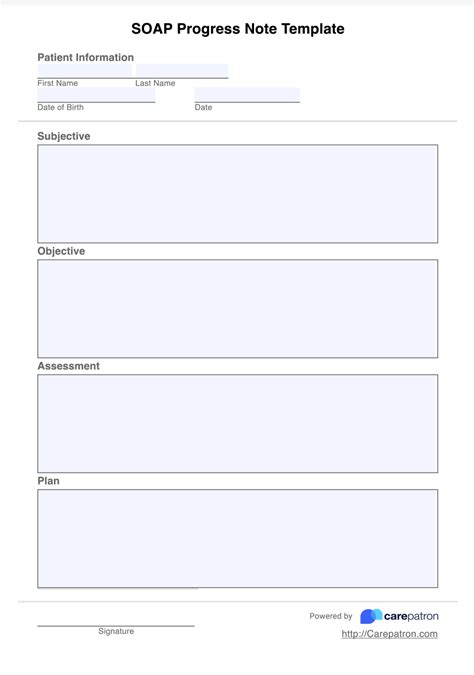
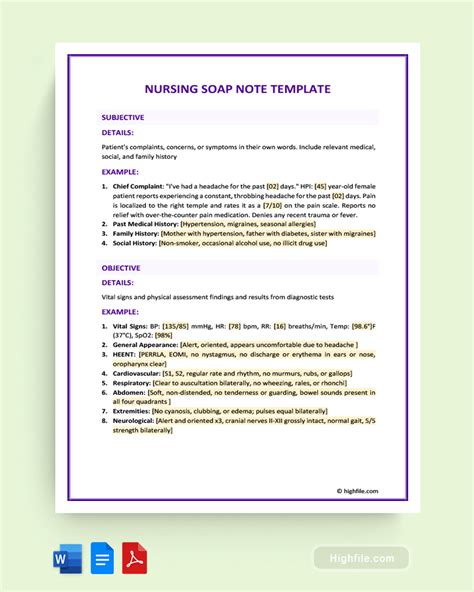
Using a SOAP note template is a straightforward process that involves the following steps:
- Subjective: Document the patient's subjective information, including their symptoms, medical history, and current condition.
- Objective: Document the patient's objective information, including their vital signs, laboratory results, and physical examination findings.
- Assessment: Document the patient's assessment, including their diagnosis, prognosis, and treatment plan.
- Plan: Document the patient's plan, including their treatment plan, follow-up appointments, and any further testing or procedures.
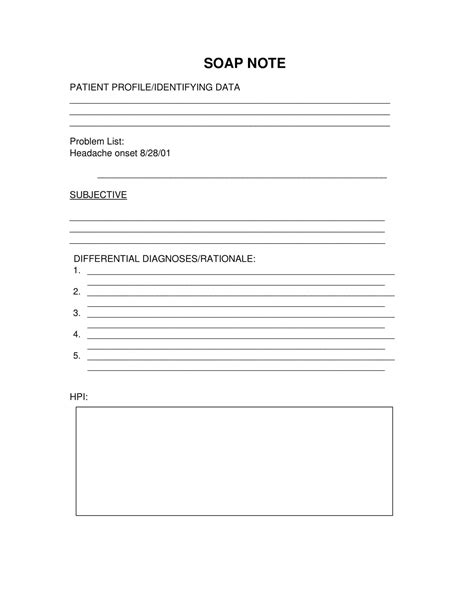
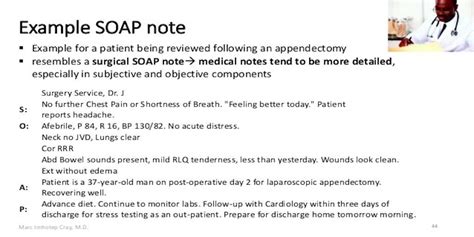
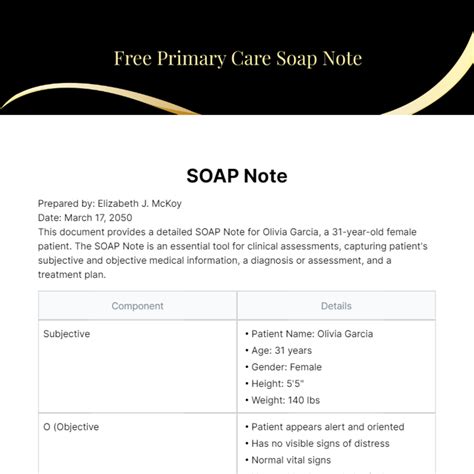
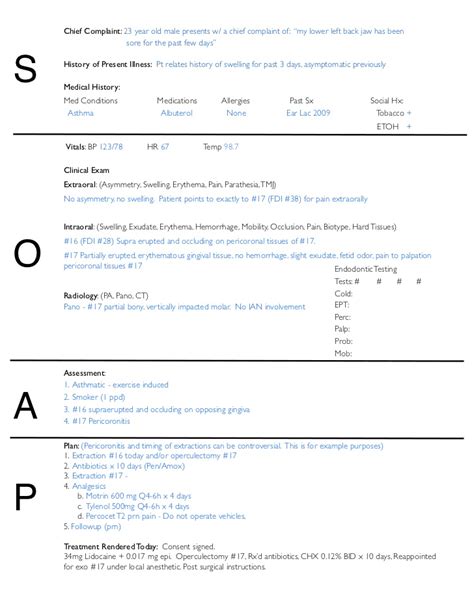
SOAP Note Template Example
Here is an example of a SOAP note template:
Subjective:
- Chief complaint: Patient complains of chest pain and shortness of breath.
- History of present illness: Patient has been experiencing chest pain and shortness of breath for the past 2 days.
- Medical history: Patient has a history of hypertension and hyperlipidemia.
- Current condition: Patient is currently experiencing chest pain and shortness of breath.
Objective:
- Vital signs: Blood pressure 140/90, pulse 100, respiratory rate 20.
- Laboratory results: Electrocardiogram (ECG) shows ST-segment elevation in leads II, III, and aVL.
- Physical examination findings: Patient has a normal body mass index (BMI) and no signs of heart failure.
Assessment:
- Diagnosis: Acute coronary syndrome (ACS).
- Prognosis: Patient has a high risk of complications, including myocardial infarction (MI) and cardiac arrhythmias.
- Treatment plan: Patient will be treated with anticoagulation therapy, beta blockers, and statins.
Plan:
- Treatment plan: Patient will be treated with anticoagulation therapy, beta blockers, and statins.
- Follow-up appointments: Patient will be seen in 2 weeks for follow-up.
- Further testing or procedures: Patient will undergo a coronary angiogram to evaluate the extent of coronary artery disease.
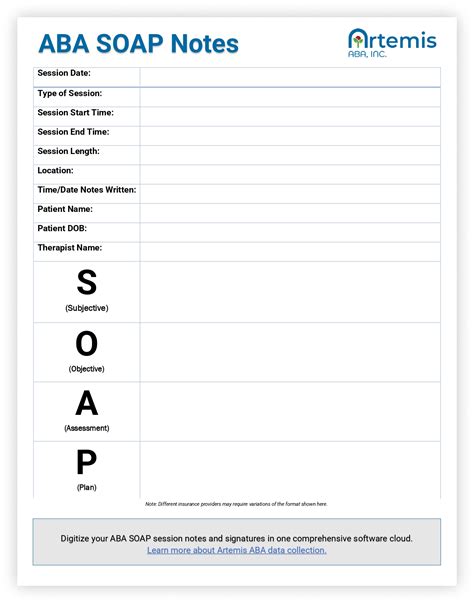
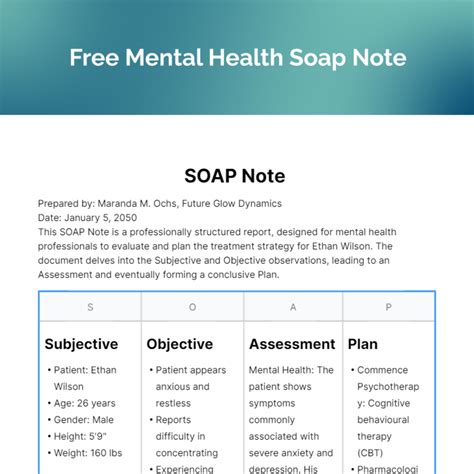
Gallery of SOAP Note Templates
SOAP Note Template Gallery


We hope this article has provided you with a comprehensive understanding of SOAP note templates and their importance in the healthcare industry. By using a SOAP note template, healthcare professionals can ensure that patient information is documented accurately and efficiently, which enables them to provide better care and make informed decisions.
