Intro
Mastering Psychiatry Soap Note Template Made Easy: Simplify patient documentation with a comprehensive guide to creating effective SOAP notes in psychiatry. Streamline your workflow with a customizable template, ensuring accurate diagnoses, treatment plans, and progress tracking. Enhance patient care with our expert tips and tricks for efficient psychiatry note-taking.
The complexity of psychiatric SOAP notes can be overwhelming, especially for medical professionals who are new to the field. A well-structured SOAP note template can help simplify the process, ensuring that all necessary information is captured and easily accessible. In this article, we will delve into the world of psychiatric SOAP notes, exploring their importance, components, and benefits. We will also provide a comprehensive template to make writing SOAP notes a breeze.
What are Psychiatric SOAP Notes?
Psychiatric SOAP notes are a type of documentation used by mental health professionals to record patient information, treatment plans, and progress. SOAP is an acronym that stands for Subjective, Objective, Assessment, and Plan. These notes serve as a vital communication tool between healthcare providers, ensuring continuity of care and facilitating collaboration.
Importance of Psychiatric SOAP Notes
Psychiatric SOAP notes play a crucial role in patient care, serving several purposes:
- They provide a comprehensive record of the patient's mental health history, symptoms, and treatment.
- They facilitate communication between healthcare providers, ensuring that all team members are aware of the patient's progress and treatment plan.
- They help track patient progress, allowing healthcare providers to adjust treatment plans as needed.
- They provide a basis for quality improvement initiatives, helping to identify areas for improvement in patient care.
Components of a Psychiatric SOAP Note
A psychiatric SOAP note typically consists of four components:
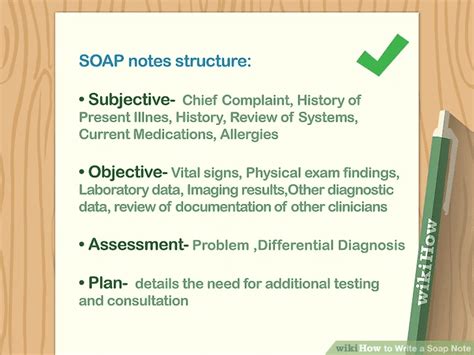
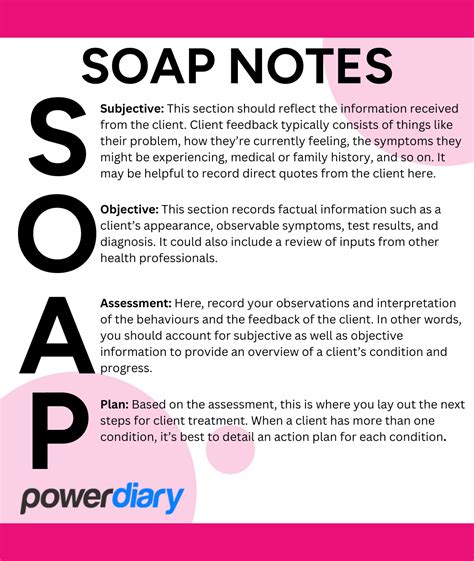
Subjective (S)
The subjective component of the SOAP note includes information provided by the patient, such as:
- Chief complaint: The patient's primary concern or reason for seeking treatment.
- History of present illness: A detailed account of the patient's symptoms, including onset, duration, and severity.
- Past medical history: A summary of the patient's relevant medical history, including previous mental health diagnoses and treatments.
Objective (O)
The objective component includes information obtained through observation, measurement, and testing, such as:
- Vital signs: The patient's temperature, blood pressure, pulse, and respiratory rate.
- Mental status examination: An assessment of the patient's mental state, including appearance, behavior, mood, and cognitive function.
- Laboratory results: The results of any laboratory tests or imaging studies.
Assessment (A)
The assessment component includes the healthcare provider's interpretation of the information gathered, including:
- Diagnosis: The healthcare provider's diagnosis of the patient's condition.
- Differential diagnosis: A list of potential diagnoses that may be considered.
- Risk assessment: An evaluation of the patient's risk for harm to themselves or others.
Plan (P)
The plan component includes the healthcare provider's plan for treatment, including:
- Medications: A list of medications prescribed, including dosage and frequency.
- Therapy: A description of any therapy or counseling recommended.
- Follow-up: A plan for follow-up appointments or monitoring.
Benefits of Using a Psychiatric SOAP Note Template
Using a psychiatric SOAP note template can have numerous benefits, including:
- Improved efficiency: A template can help healthcare providers quickly and easily document patient information.
- Enhanced organization: A template can help ensure that all necessary information is captured and easily accessible.
- Better communication: A template can facilitate communication between healthcare providers, ensuring that all team members are aware of the patient's progress and treatment plan.
- Reduced errors: A template can help reduce errors by ensuring that all necessary information is captured and accurately documented.
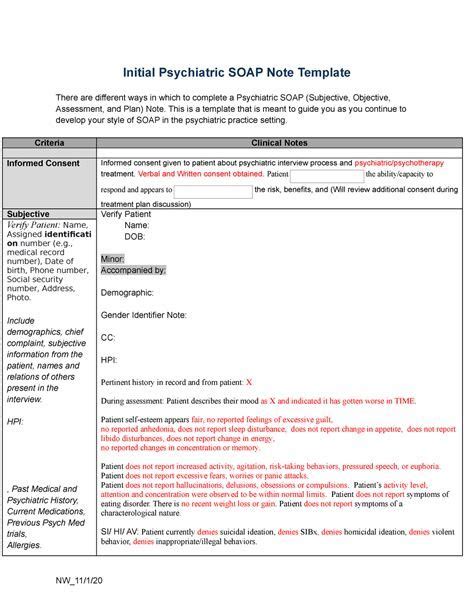
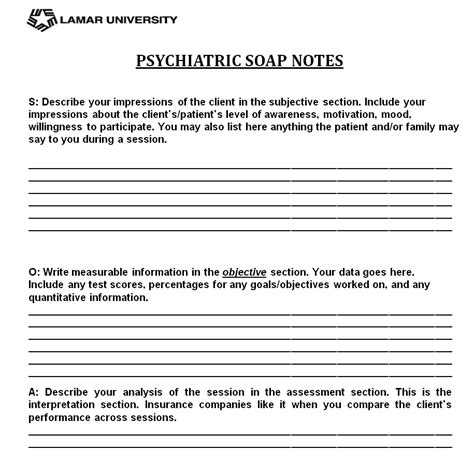
Psychiatric SOAP Note Template
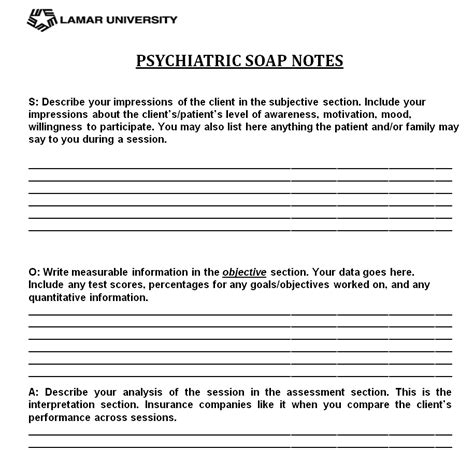
Here is a comprehensive psychiatric SOAP note template that you can use:
Subjective
- Chief complaint: _____________________________________________________
- History of present illness: _____________________________________________________
- Past medical history: _____________________________________________________
Objective
- Vital signs:
- Temperature: _______________________
- Blood pressure: _______________________
- Pulse: _______________________
- Respiratory rate: _______________________
- Mental status examination:
- Appearance: _______________________
- Behavior: _______________________
- Mood: _______________________
- Cognitive function: _______________________
- Laboratory results: _____________________________________________________
Assessment
- Diagnosis: _____________________________________________________
- Differential diagnosis: _____________________________________________________
- Risk assessment: _____________________________________________________
Plan
- Medications:
- Medication: _______________________
- Dosage: _______________________
- Frequency: _______________________
- Therapy:
- Type of therapy: _______________________
- Frequency: _______________________
- Follow-up:
- Next appointment: _______________________
- Follow-up plan: _____________________________________________________
Gallery of Psychiatric SOAP Note Templates
Psychiatric SOAP Note Templates
In conclusion, a well-structured psychiatric SOAP note template can help simplify the documentation process, ensuring that all necessary information is captured and easily accessible. By using the template provided, healthcare providers can improve efficiency, enhance organization, and facilitate communication. We hope this article has been informative and helpful in making psychiatric SOAP notes a breeze.
