Intro
Master the art of documenting patient care with a well-structured Soap Note Template in Word. Learn the 7 essential elements to include for accurate and efficient charting. Discover how to create a comprehensive template that covers Subjective, Objective, Assessment, and Plan, while incorporating relevant medical history, diagnosis, and treatment plans.
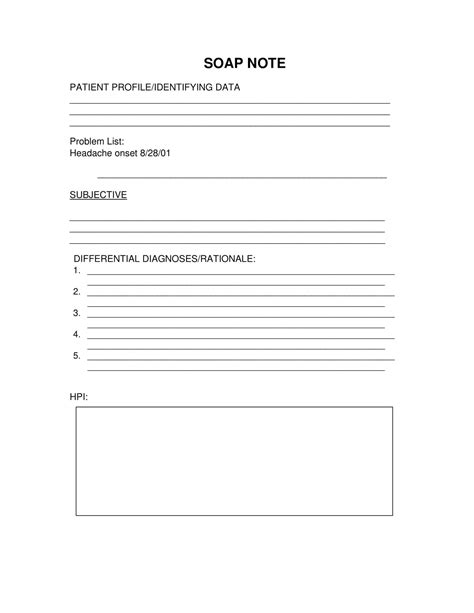
As a healthcare professional, taking accurate and detailed notes is crucial for providing high-quality patient care. A SOAP note template in Word is a valuable tool for organizing your thoughts and ensuring that you capture all the essential information during patient encounters. In this article, we will explore the 7 essential elements of a SOAP note template in Word, along with some practical examples and tips to help you create your own template.
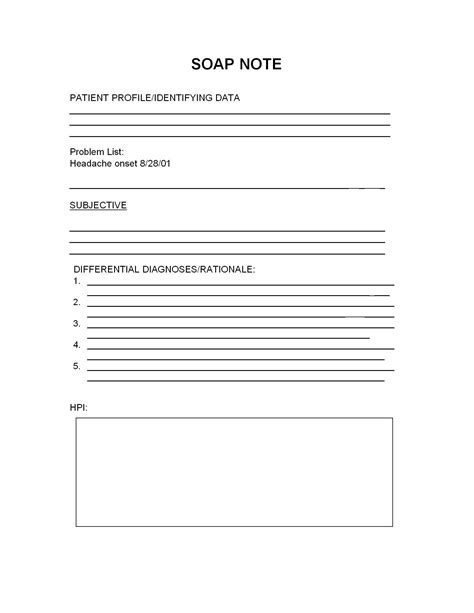
What is a SOAP Note Template?
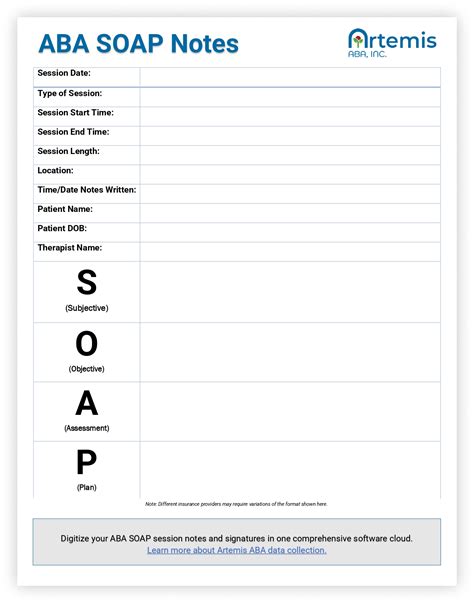
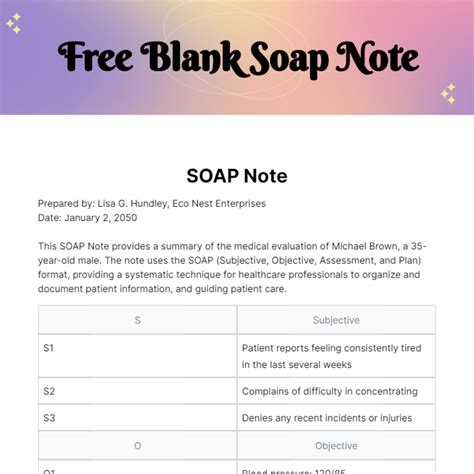
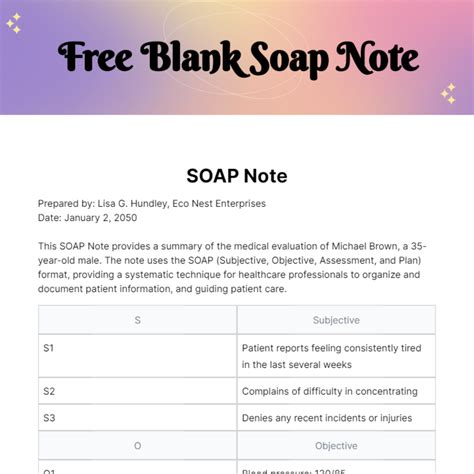
A SOAP note template is a pre-designed document that helps healthcare professionals take structured notes during patient encounters. The SOAP acronym stands for Subjective, Objective, Assessment, and Plan, which are the four main sections of a SOAP note. These templates are widely used in healthcare settings, including hospitals, clinics, and private practices, to ensure consistency and accuracy in patient documentation.
Benefits of Using a SOAP Note Template
Using a SOAP note template in Word offers several benefits, including:
- Improved documentation accuracy and completeness
- Enhanced patient care through better organization and analysis of patient data
- Increased efficiency and reduced time spent on note-taking
- Improved communication among healthcare team members
- Reduced risk of medical errors and improved patient safety
The 7 Essential Elements of a SOAP Note Template
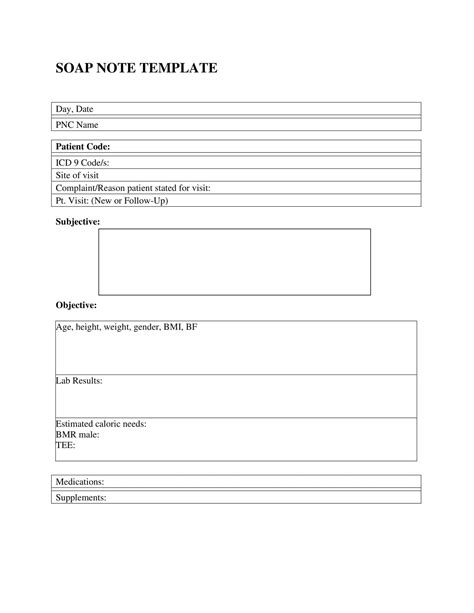
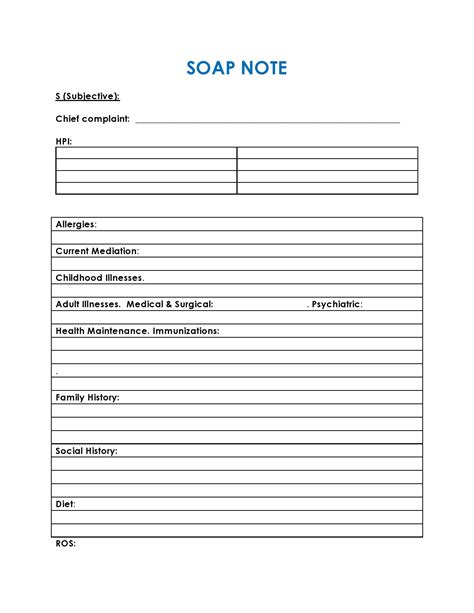
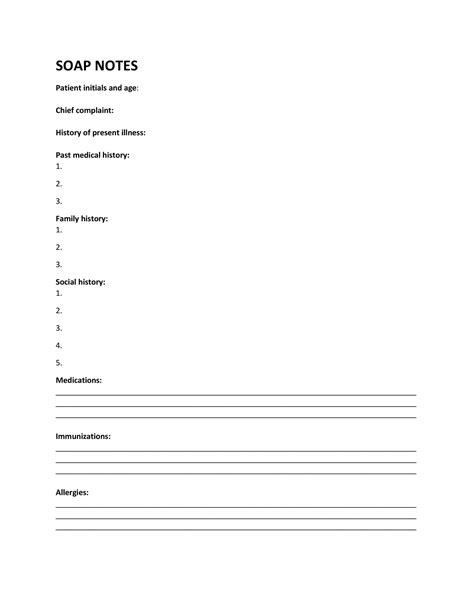
While SOAP note templates may vary depending on the specific healthcare setting or specialty, there are 7 essential elements that should be included in every template:
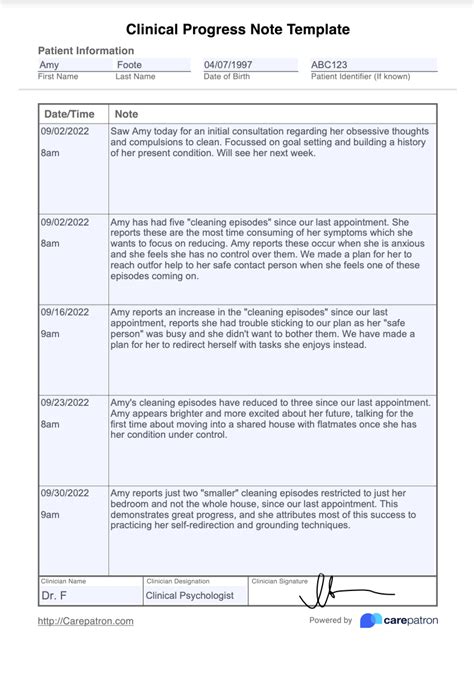
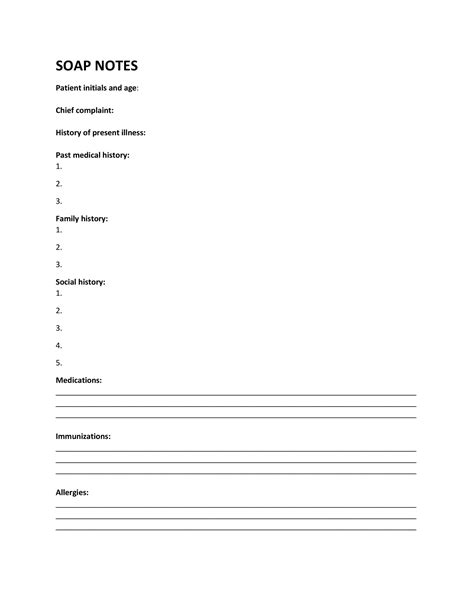
1. Patient Information
This section should include basic patient demographics, such as name, date of birth, medical record number, and contact information.
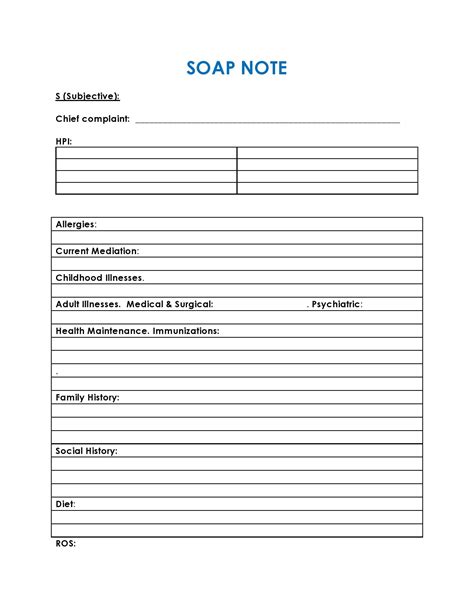
2. Subjective Data
This section should capture the patient's subjective complaints, symptoms, and concerns. This information is typically gathered through patient interviews and should be recorded in the patient's own words.

3. Objective Data
This section should include objective data gathered through physical examination, laboratory results, and other diagnostic tests.

4. Assessment
This section should summarize the patient's condition, including any diagnoses, symptoms, and concerns.
5. Plan
This section should outline the plan of care, including any treatments, medications, or follow-up appointments.
6. Progress Notes
This section should provide space for documenting progress notes, including any changes in the patient's condition or treatment plan.
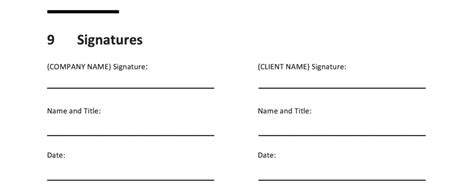
7. Signature and Date
Finally, every SOAP note template should include space for the healthcare provider's signature and date.
Creating Your Own SOAP Note Template in Word
Creating your own SOAP note template in Word is a straightforward process. Here are some steps to follow:
- Open a new Word document and create a table with the 7 essential elements as headings.
- Customize the template to fit your specific needs and healthcare setting.
- Use clear and concise language in your template.
- Test your template with a sample patient scenario to ensure it is effective.
SOAP Note Template in Word Image Gallery
Conclusion
A SOAP note template in Word is a valuable tool for healthcare professionals to take accurate and detailed notes during patient encounters. By including the 7 essential elements outlined in this article, you can create a comprehensive and effective template that improves patient care and reduces medical errors. Remember to customize your template to fit your specific needs and healthcare setting, and test it with a sample patient scenario to ensure its effectiveness.
