Intro
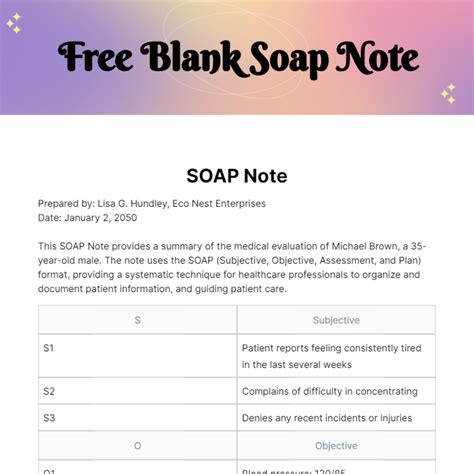
Streamline your documentation with a comprehensive blank soap note template. Learn the 5 essential components, including patient information, subjective and objective data, assessment, and plan, to ensure accurate and efficient note-taking. Discover how to create a template that meets your healthcare needs, boosts productivity, and improves patient care with our expert guide.
Maintaining accurate and detailed medical records is crucial for healthcare professionals to provide high-quality patient care. A blank soap note template is a valuable tool that helps medical professionals document patient information in a structured and organized manner. In this article, we will explore the five essential components of a blank soap note template and their significance in medical documentation.
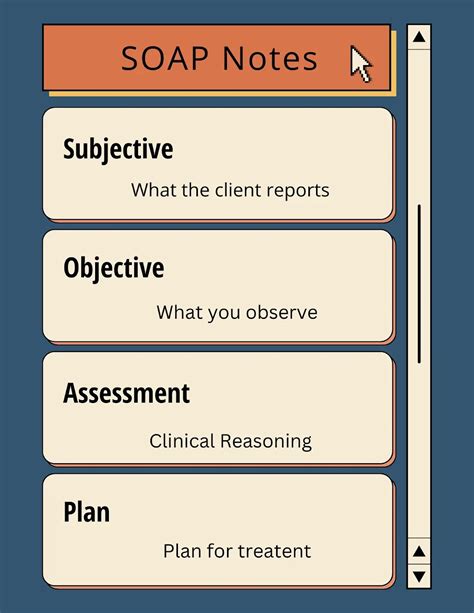
The Importance of SOAP Notes
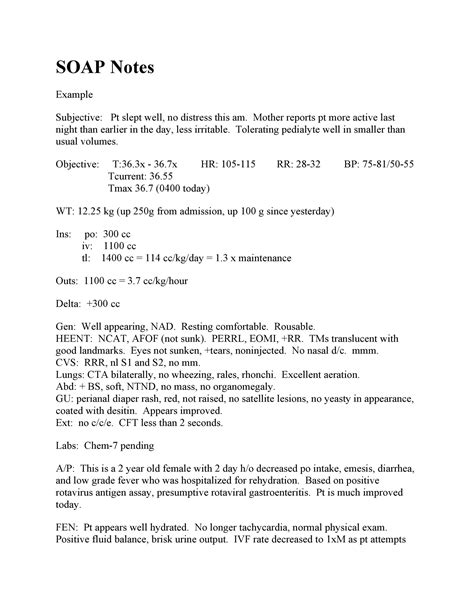
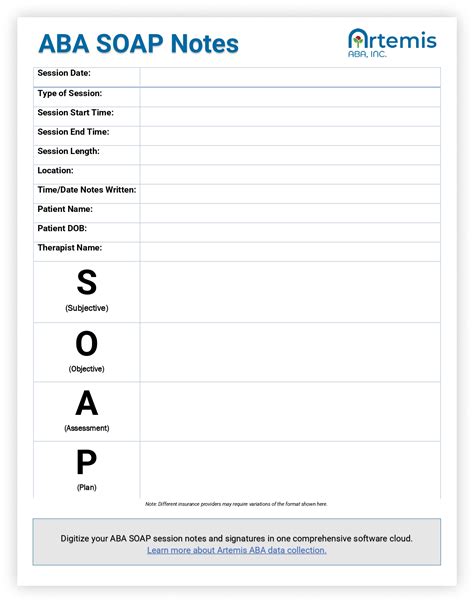
SOAP notes, an acronym for Subjective, Objective, Assessment, and Plan, are a widely accepted method of documenting patient information in the medical field. They provide a standardized framework for healthcare professionals to record patient data, facilitating effective communication and continuity of care. A blank soap note template serves as a starting point for medical professionals to create comprehensive and accurate patient records.
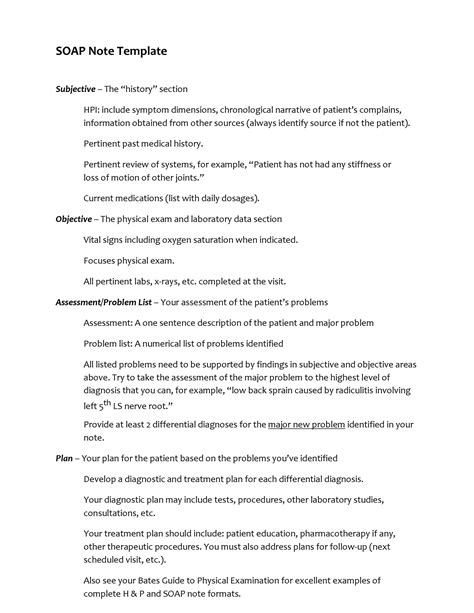
Component 1: Subjective (S)
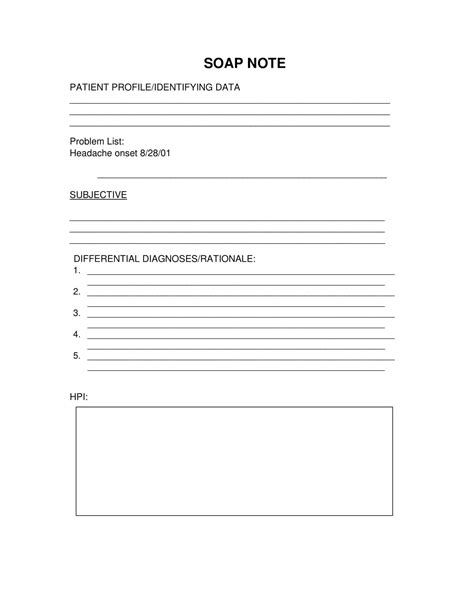
The subjective component of a soap note template captures the patient's personal account of their symptoms, medical history, and concerns. This section includes:
- Chief complaint: A brief statement of the patient's primary concern
- History of present illness (HPI): A detailed description of the patient's symptoms and their duration
- Review of systems (ROS): A comprehensive review of the patient's bodily systems and any symptoms or concerns related to them
- Past medical history (PMH): A record of the patient's previous medical conditions, surgeries, and hospitalizations
Component 2: Objective (O)
The objective component of a soap note template records the healthcare professional's observations and findings from the physical examination, diagnostic tests, and other objective data. This section includes:
- Vital signs: A record of the patient's temperature, blood pressure, pulse, respiratory rate, and oxygen saturation
- Physical examination findings: A description of the patient's physical condition, including any abnormalities or notable findings
- Laboratory and diagnostic test results: A record of the results from laboratory tests, imaging studies, and other diagnostic procedures
Component 3: Assessment (A)
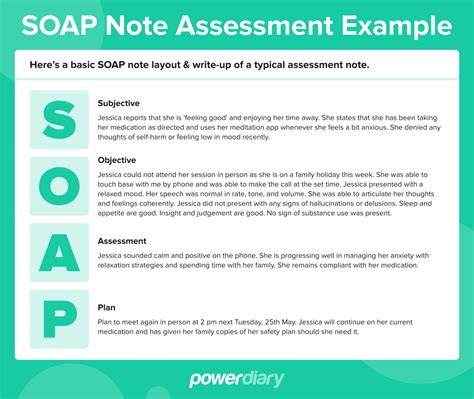
The assessment component of a soap note template summarizes the healthcare professional's interpretation of the patient's condition and identifies any relevant diagnoses or issues. This section includes:
- Diagnosis: A statement of the patient's medical condition or diagnosis
- Differential diagnosis: A list of potential alternative diagnoses
- Problem list: A record of the patient's active medical problems and concerns
Component 4: Plan (P)
The plan component of a soap note template outlines the healthcare professional's recommendations for the patient's care and management. This section includes:
- Treatment plan: A description of the planned interventions, medications, or therapies
- Diagnostic plan: A plan for further diagnostic testing or evaluation
- Follow-up plan: A plan for the patient's follow-up care and monitoring
Component 5: Additional Information
The additional information component of a soap note template provides space for healthcare professionals to record any additional relevant information, such as:
- Allergies: A record of the patient's known allergies
- Medications: A list of the patient's current medications
- Family and social history: A record of the patient's family and social history, including any relevant medical information
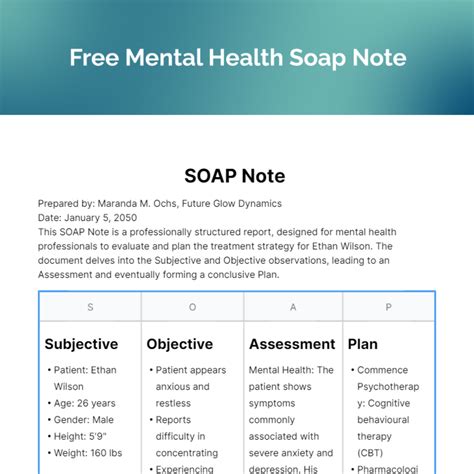
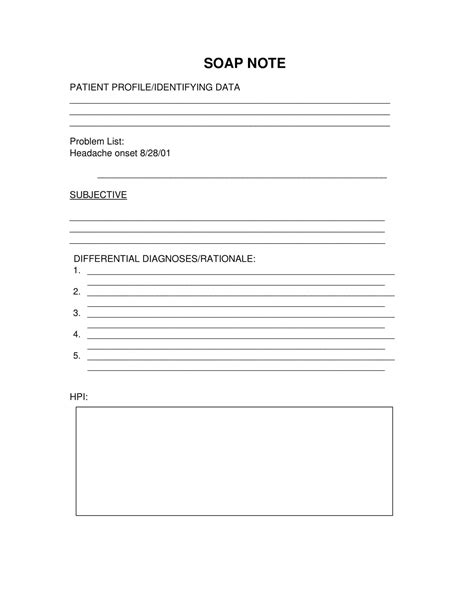
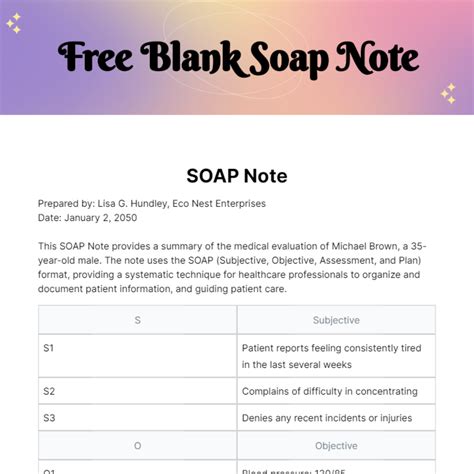
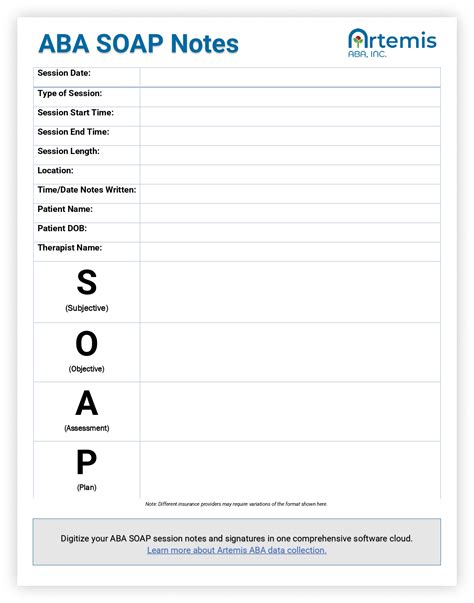
Gallery of SOAP Note Templates
SOAP Note Template Image Gallery
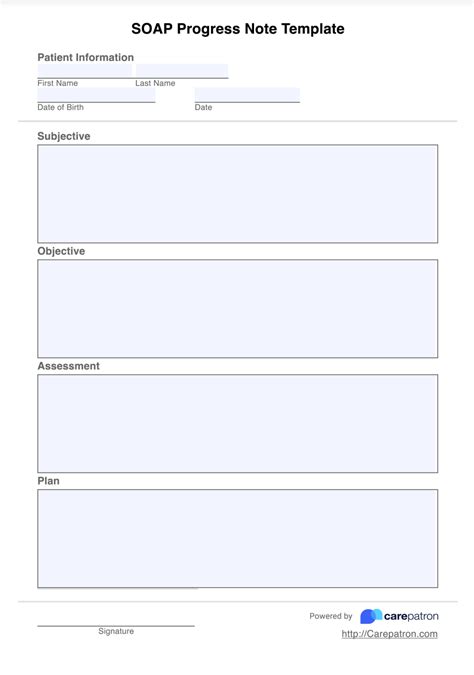
By including these five essential components, a blank soap note template provides a comprehensive framework for healthcare professionals to document patient information and create accurate and detailed medical records. The use of a soap note template ensures that healthcare professionals can efficiently and effectively communicate patient information, promoting high-quality patient care and continuity of care.
