Intro
Discover the complexities of Diabetes Insipidus, a rare endocrine disorder that affects the bodys ability to regulate fluids. Learn about the causes, symptoms, and treatment options for this chronic condition, including hormone replacement therapy and lifestyle modifications, to manage excessive thirst and urination.
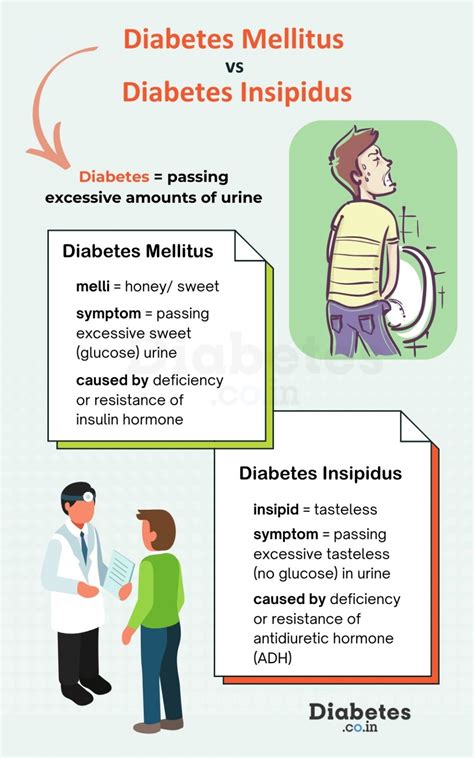
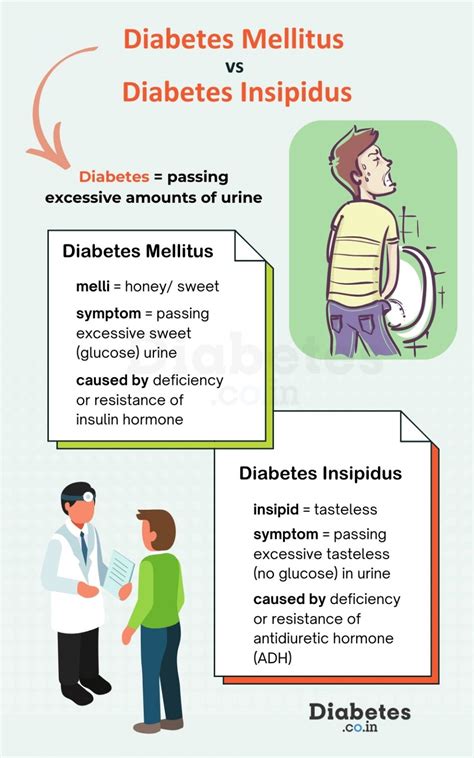
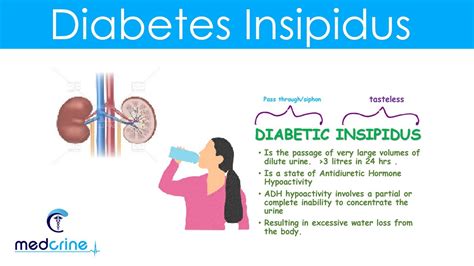
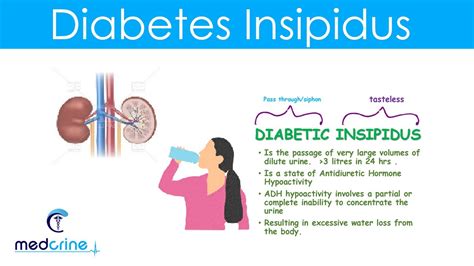
Diabetes insipidus is a rare endocrine disorder that affects the body's ability to regulate fluids. Unlike diabetes mellitus, which is a condition characterized by high blood sugar levels, diabetes insipidus is a disorder that affects the kidneys' ability to reabsorb water. This results in the production of large amounts of diluted urine, which can lead to dehydration if left untreated. In this article, we will delve into the world of diabetes insipidus, exploring its causes, symptoms, diagnosis, and treatment options.
What is Diabetes Insipidus?
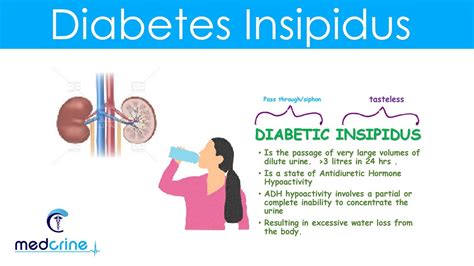
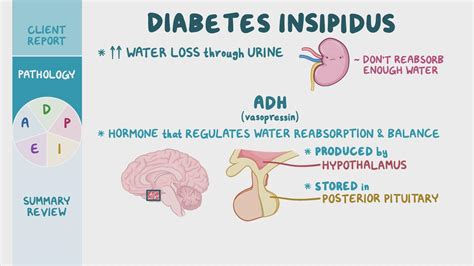
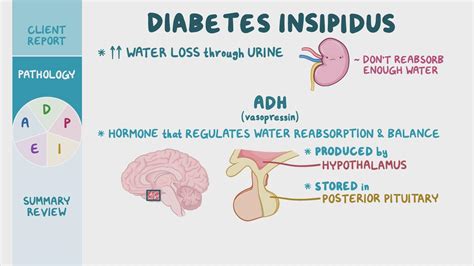
Diabetes insipidus is a condition characterized by the excessive production of urine, resulting in dehydration. The disorder is caused by a deficiency in antidiuretic hormone (ADH), also known as vasopressin, which is produced by the hypothalamus in the brain and stored in the posterior pituitary gland. ADH plays a crucial role in regulating the amount of water in the body by controlling the reabsorption of water in the kidneys.
Types of Diabetes Insipidus
There are four types of diabetes insipidus, each with distinct causes and symptoms.
- Central Diabetes Insipidus: This type of diabetes insipidus is caused by a deficiency in ADH production, often due to damage to the hypothalamus or pituitary gland.
- Nephrogenic Diabetes Insipidus: This type of diabetes insipidus is caused by a defect in the kidneys' ability to respond to ADH, resulting in the inability to reabsorb water.
- Gestational Diabetes Insipidus: This type of diabetes insipidus occurs during pregnancy and is caused by the destruction of ADH by an enzyme produced by the placenta.
- Dipsogenic Diabetes Insipidus: This type of diabetes insipidus is caused by a defect in the thirst mechanism, leading to excessive water intake and production of diluted urine.
Symptoms of Diabetes Insipidus
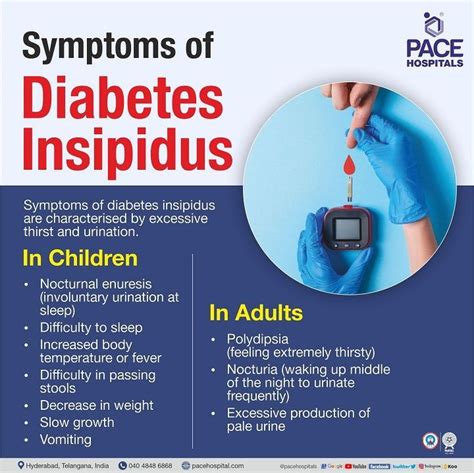
The symptoms of diabetes insipidus can vary depending on the type and severity of the disorder. Common symptoms include:
- Polyuria: Excessive production of urine, often resulting in the production of large amounts of diluted urine.
- Polydipsia: Excessive thirst, which can lead to dehydration if left untreated.
- Dehydration: Dehydration can occur if the body is unable to reabsorb water, leading to symptoms such as dry mouth, fatigue, and headaches.
- Nocturia: Frequent urination at night, which can disrupt sleep patterns and lead to fatigue.
Diagnosis of Diabetes Insipidus
Diagnosing diabetes insipidus can be challenging, as the symptoms can be similar to those of other disorders. A diagnosis of diabetes insipidus is typically made based on a combination of the following:
- Medical History: A thorough medical history is taken to rule out other conditions that may be causing the symptoms.
- Physical Examination: A physical examination is performed to assess the patient's overall health and look for signs of dehydration.
- Laboratory Tests: Laboratory tests, such as urine and blood tests, are performed to assess the patient's kidney function and hormone levels.
- Imaging Studies: Imaging studies, such as MRI or CT scans, may be performed to assess the pituitary gland and hypothalamus.
Treatment of Diabetes Insipidus
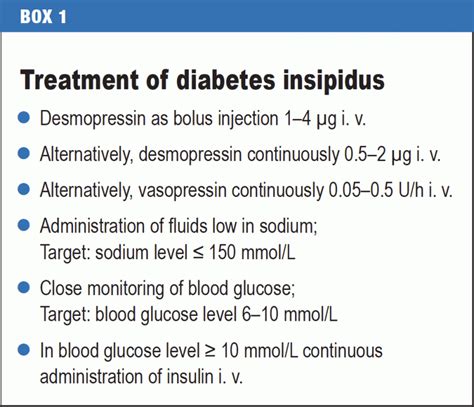
Treatment of diabetes insipidus depends on the type and severity of the disorder. Treatment options may include:
- Hormone Replacement Therapy: Hormone replacement therapy may be prescribed to replace the deficient hormone, ADH.
- Desmopressin: Desmopressin is a synthetic hormone that is used to treat central diabetes insipidus.
- Thiazide Diuretics: Thiazide diuretics may be prescribed to help the kidneys reabsorb water.
- Lifestyle Changes: Lifestyle changes, such as increasing fluid intake and avoiding foods that can exacerbate dehydration, may be recommended.
Living with Diabetes Insipidus
Living with diabetes insipidus requires careful management of the disorder to prevent dehydration and other complications. Patients with diabetes insipidus should:
- Stay Hydrated: Patients should drink plenty of water to stay hydrated, especially in hot weather or during exercise.
- Monitor Urine Output: Patients should monitor their urine output to ensure that they are producing a normal amount of urine.
- Avoid Dehydration: Patients should avoid dehydration by drinking water regularly and avoiding foods that can exacerbate dehydration.
- Follow Treatment Plan: Patients should follow their treatment plan carefully to manage their symptoms and prevent complications.
Diabetes Insipidus Image Gallery

If you or a loved one has been diagnosed with diabetes insipidus, it is essential to work closely with a healthcare provider to manage the disorder and prevent complications. By staying hydrated, monitoring urine output, and following treatment plans, individuals with diabetes insipidus can lead active and healthy lives.
